 Annie Spratt/Unsplash
Annie Spratt/UnsplashHave you ever sat with a cup of tea at the end of a weeding session, with a feeling close to happiness? Or returned from the local garden centre with a bag of potting mix and some plants – and soon the sight of your newly planted herbs or flowers makes your heart feel inexplicably lighter?
Perhaps you’re in hospital recovering from surgery, as I was only a little time ago. I regained consciousness in an advanced recovery unit, a dimly lit space with no windows where everything felt slightly surreal and too intense.
I was receiving the best possible care, yet I had a desperate sense of having been cut loose from my life, and even from my body, as it was monitored and medicated throughout the night. Who knows where things might go from here, I thought. Yet I almost didn’t care.
In the morning, I was wheeled away to a room on an upper floor. It was a space flooded with natural light and with a view of a wintry, cloudy sky and distant treetops.
When a friend arrived with a posy of flowers, I found myself smiling for the first time since leaving home. As well as the pleasure of her company, there was a surge of delight at the presence of flowers. Their soft colours soothed something in me that had been clutched tight in fear since my first glimpse of the stark, frankly terrifying operating theatre.
A history of healing
Perhaps now, more than ever, we could all use some green relief, as we deal with a world that seems to only grow more anxiety-inducing and uncertain.
In May, Australians will vote in what has been called “the cost-of-living election”. Housing prices (and homelessness) have soared, too, with one study putting the rise in housing value between March 2020 and February 2024 at 32.5%.
Elsewhere, war rages in Ukraine, Gaza, and other countries, and the world order is wobbling in the wake of the US elections – particularly this week, when Donald Trump’s tariffs sparked a stock market crash not seen since COVID (until he changed his mind yesterday and it recovered) and led to predictions of a recession.
What evidence is there that the natural world can have a healing effect?
 Green relief can help us deal with an uncertain world. Annie Spratt/Unsplash
Green relief can help us deal with an uncertain world. Annie Spratt/UnsplashIn most cultures throughout history, medicine and botany have been closely entwined, and gardens have been associated with healing the body, mind, and spirit. From around the 4th century BCE, Greece had healing centres known as “asclepieia”, after the god of medicine, Asclepius.
In medieval Europe, monasteries kept medicinal gardens. In England, hospitals and asylums were set within landscaped grounds in the belief the tranquillity of the setting played an important role in lifting patients’ mood. Both male and female inmates of 19th-century asylums often worked in the gardens, in what was seen as a healing process administered by the place itself.
Inevitably, the creep of urbanisation saw the garden landscapes of many such institutions greatly reduced, yet the health benefits to patients of connecting with nature remains undiminished.
Flowers and healing
An explanation for the uplifting effect of those flowers in my hospital room may be found in numerous studies that have shown, post-surgery, patients in rooms with plants and flowers have shorter recovery times, require fewer analgesics, and experience lower levels of anxiety. Partly, it is a response to beauty.
As psychiatrist Sue Stuart-Smith writes in The Well Gardened Mind, the human response to beauty involves brain pathways “associated with our dopamine, serotonin, and endogenous opioid systems and damp down our fear and stress responses”. She continues: “Beauty calms and revitalises us at the same time.” We humans have an affinity for patterns and order, she writes. “The simple geometrics we find in nature are perhaps most concentrated and compelling in the beauty of a flower’s form.”
There has been a trend towards banning flowers from hospital wards, on health grounds. Reasons include a suspicion bacteria lurk in the flower water, as well as safety concerns around patients or nursing staff knocking over vases during night shifts.
Florence Nightingale, in her Notes on Nursing, commented on the beneficial effects of flowers on her patients. She added that they recovered more quickly if they could spend time outside, or at least had a room with adequate natural light. “It is a curious thing to observe how almost all patients lie with their faces turned to the light, exactly as plants always make their way towards the light.” Even if lying on a particular side caused pain, patients still preferred it, Nightingale noted – because “it is the side towards the window”.
Our compulsion to turn towards the natural world is known as “biophilia”. The term was first coined in the 1960s, by German–American social psychologist and psychoanalyst, Erich Fromm. He described it as “the passionate love of life and all that is alive”, speculating that our separation from nature brings about a level of unrecognised distress.
In the 1980s, biologist and ecologist Edward O. Wilson, in his book Biophilia, asserted that all humans share an affinity with the natural world. “The urge to affiliate with other forms of life is to some degree innate,” he wrote.
In hospital, as my body began its tentative recovery from the shock of surgery, I remembered a line popularly attributed to the French Impressionist painter, Claude Monet: “What I need most are flowers, always, and always.” Through his paintings, notably his studies of waterlilies, and the garden he established at Giverny, which welcomes visitors to the present day, Monet’s flowers continue to calm and revive us with their transcendent beauty.
Perhaps the simplest way to forge a connection with nature lies in our own suburban gardens, if we are lucky enough to have them. Aside from the pleasure of creating pleasing spaces, contact with the soil bacteria Mycobacterium vaccae has been shown to trigger the release of serotonin in the brain. Serotonin, a natural antidepressant, strengthens the immune system. An added bonus is that when we harvest edible plants, our brain releases dopamine, flushing our systems with a gentle rush of satisfaction and pleasure.
Regular doses of serotonin and dopamine were never more needed than during the pandemic, when lockdowns unleashed a sudden fervour for gardening.
In her book The Garden Against Time, Olivia Laing writes that “over the course of 2020, three million people in Britain began to garden for the first time, over half of them under forty-five”. And it wasn’t just in Britain, where garden centres ran out of plants and compost as people set to work transforming the spaces where they were confined.
Australia experienced a similar surge in interest, with the ABC reporting sales of herb and vegetable plants shot up 27%, joining toilet paper and pasta on the list of panic buys. In the United States, Laing writes, 18.3 million people started gardening, “many of them millennials”. American seed company W. Atlee Burpee “reported more sales in the first March of lockdown than at any other time in its 144-year history”.
Laing writes:
crouched on the threshold of unimaginable disaster, death toll soaring, no cure in sight – it was reassuring to see the evidence of time proceeding as it was meant to, seeds unfurling, buds breaking, daffodils pushing through the soil; a covenant of how the world should be and might again.
 In 2020, sales of herb and vegetable plants soared 27% in Australia. Annie Spratt/Unsplash
In 2020, sales of herb and vegetable plants soared 27% in Australia. Annie Spratt/UnsplashIt is precisely this “evidence of time proceeding as it was meant to” that has the power to hold humans calmly in place. We may imagine we want more than this from life; despising dullness, we think we crave excitement and change. But given the option, few would choose to wake to an Orwellian “bright cold day in April” to find “the clocks were striking thirteen”, which is how it felt during those nightmarish early days of the COVID-19 crisis.
Life on earth does still feel somewhat bright and cold, its future somewhat bleak; it is as if Orwell’s dystopian vision is at last catching up with us.
Who would believe an activity so apparently humble as gardening could come to the rescue of millions of stressed and fearful people? Yet gardeners seem to know this instinctively.
Tending ourselves
In the book In Kiltumper: a Year in an Irish Garden, co-written with her husband, Niall Williams, Irish writer and gardener Christine Breen describes the ordeal of undergoing cancer treatment through the Irish healthcare system. Following an oncology appointment in Galway, the couple drives home towards west Clare, or as Christine puts it: “back to the garden, where there is safety”.
Christine’s husband Niall confirms that, although the medical community might dismiss the healing power of working in a garden as “airey-fairy”, in Christine’s case, even while weak from chemotherapy, “going about the flower beds, trying to do exactly the same work she had always done” meant continuity.
It represented “carrying on living, because that is one of the prime lessons any garden teaches you: the garden grows on”. He speculates that after many years together, garden and gardener become one: “when we tend it, we tend some part of ourselves”.
If we know this, we too often forget. Consequently, garden centres rarely top the list of most desirable destinations, and gardening has been traditionally represented as fussy and domestic. Weeding and mowing are seen as chores that, if possible, are to be avoided.
 When we tend a garden, we tend some part of ourselves. Benjamin Combs/Unsplash
When we tend a garden, we tend some part of ourselves. Benjamin Combs/UnsplashIn her book Why Women Grow, Alice Vincent writes that gardening has “so many associations, of neatness and nicety; a prissiness that feels deeply removed […] from the sex and death and life on show in every growing thing.” She writes: “When we garden, we change how a small part of the world works.”
Doubtless, it was this sense of being able to change one’s world, of seizing control, that appealed to so many of us during the pandemic. And if we got our hands into the soil, we were rewarded with much-needed infusions of serotonin.
In literature, too, people suffering physically or mentally, or both, have often sought refuge or found solace in a garden.
For many readers, their first encounter with the transformative nature of gardening was Frances Hodgson Burnett’s classic children’s book, The Secret Garden. In it, a spoilt yet neglected child, Mary Lennox, is orphaned in India when her parents and their servants succumb to cholera. She is bundled off to Yorkshire, England, to a daunting atmosphere of secrecy and neglect at Misselthwaite Manor, into the care of an uncle she has never met. There, Mary soon discovers the key to a garden that has been locked for years following her aunt’s death.
In her efforts to restore life to the neglected garden, Mary herself is restored, gradually shedding the lonely, helpless persona of her Indian childhood. When she discovers the manor’s other tightly held secret – her sickly, bedridden cousin, Colin – Mary manages to get him, too, out of the house and into the garden. The outcome is healing for the children, and eventually for Mary’s grieving uncle.
Green prescriptions
For a real-life example of green relief, in The Well Gardened Mind, Sue Stuart-Smith describes how her grandfather – a submariner in the first world war – was taken prisoner during the Gallipoli campaign. After a series of brutal labour camps in Turkey, the last of them in a cement factory, he eventually escaped.
But after the long journey home he was so severely malnourished he was given only a few months to live. Crucial to regaining his health was the devoted nursing by his fiancée, followed by a year-long horticultural course set up to rehabilitate ex-servicemen.
A psychiatrist as well as a gardener, Stuart-Smith writes of the therapeutic effects of working with our hands in a protected space. She describes how gardening allows our inner and outer worlds “to coexist free from the pressures of everyday life”.
Gardens, she writes, are an “in-between space which can be a meeting place for our innermost, dream-infused selves and the real physical world”. In a garden, we are able to hear and process our own, sometimes turbulent, thoughts.
In 1986, after being diagnosed HIV positive, the English artist and filmmaker Derek Jarman retreated to the Kent coast near the nuclear power station at Dungeness. In The Garden Against Time, Olivia Laing writes that at Prospect Cottage, Jarman
began with stones, not plants: the grey flints he called dragon’s teeth, revealed by the tide on morning walks.
 Prospect Cottage, former home of filmmaker Derek Jarman, Dungeness. Poliphilo/Wikimedia Commons, CC BY
Prospect Cottage, former home of filmmaker Derek Jarman, Dungeness. Poliphilo/Wikimedia Commons, CC BYGradually he established a garden in the inhospitable soil, seeing it as “a therapy and a pharmacopoeia” – and “a place of total absorption”.
It was this capacity to slow or stop time, as much as its wild and sportive beauty, that made it such a paradise-haunted place.
The pandemic spread waves of turbulence across the globe. In April 2021, as part of its post-COVID recovery plan, the government of the United Kingdom launched a two-year green social prescription pilot.
Project-managed by the National Health Service, the program worked across seven test sites: areas disproportionately affected by the pandemic. These included people living in deprived areas and people with mental health conditions, many of them from ethnic minority communities.
Over the course of the two-year program, more than 8,500 people were referred to a green social prescribing activity. Green networks were established in all seven test sites. Findings showed positive improvements in mental health and wellbeing – and green social prescribing is ongoing, proof of the program’s lasting impact.
In recent times, doctors in some countries are writing green prescriptions, rather than scripts for medication. And not just for mental health problems, but for physical conditions such as high blood pressure, diabetes and lung diseases.
In the late 1990s, New Zealand became one of the first countries where GPs used green prescriptions to encourage patients to increase their levels of physical activity. Japanese clinicians have been advocating “shinrin-yoku”, or forest bathing for decades. In Finland, with its long dark winters, five hours a month is regarded as a “minimum dose” of contact with nature.
 New Zealand was one of the first countries where GPs used green prescriptions to encourage patients to boost their physical activity. Kari Kittlaus/Pexels
New Zealand was one of the first countries where GPs used green prescriptions to encourage patients to boost their physical activity. Kari Kittlaus/PexelsAside from the physical benefits, time spent in a garden can provide a mood boost for those of us who feel oppressed by calendars, and by clock time’s relentless march. In her 2018 memoir Life in the Garden, Penelope Lively writes:
To garden is to elide past, present and future; it is a defiance of time. You garden today for tomorrow, the garden mutates from season to season, always the same but always different.
Perhaps no group of people stands in greater need of time-defiance than those of us entering the final decades of our lives. Time is short, and we know it. But as now 92-year-old Lively wrote seven years ago: “A garden is never just now; it suggests yesterday and tomorrow; it does not allow time its steady progress.”
 A garden is a ‘defiance of time’. Pexels
A garden is a ‘defiance of time’. PexelsGardening as defiance
My mother pottered in her garden until she was in her early 90s, pruning roses, pulling weeds, planting annuals and throwing down fertiliser. She’d wrestle her walker across the lawn to perch on its seat while she did the watering, before retreating to an armchair in the back room of her house, from where she could admire her achievements.
Gardening in extreme old age was, for her, an act of defiance – against time, and against her children, who nagged about the possibility of a fall and insisted she wear an emergency call button. It was a defiance, too, of the common view that old people should relinquish their homes with gardens and move into something more manageable.
On the face of it, not having a garden to maintain in old age makes perfect sense, but it may come at the expense of our human impulse to seek connection with living things, specifically those in the natural world. So ingrained is our instinct to connect with nature, it appears to survive even when other systems and connections have broken down.
A friend whose Alzheimer’s-afflicted husband is in residential care reports he is constantly finding odd containers, filling them with soil, and planting cuttings gathered from the care home’s garden. He crams them onto his windowsill, even planting in teacups when there is nothing else to hand.
Accustomed to gardening throughout his adult life, his impulse to work with living things persists in defiance of dementia. My friend reflects her mother used to do the same, only she would take pieces from the home’s fake indoor plants, then complain bitterly when they did not grow.
In the care facility my friend visits daily, women pick flowers in the grounds to decorate their walkers, and when there are no flowers they’ll use pictures of flowers cut from magazines. Cutting out paper flowers seems like the action of someone whose garden has been lost, but who still feels a powerful desire to connect with beauty and the natural world.
Imagined gardens
The theories of 20th-century historian Theodore Roszak, in his book The Voice of The Earth, founded the ecopsychology movement.
He believed “humans connect with nature through the ecological unconscious, which is the core of human identity”. Human nature, he wrote, is “densely embedded in the world we share with animal, vegetable, mineral”. He believed reconnecting with nature helps people become more aware of their connection to all living things.
So what are we to do if the garden has been lost?
The French writer Colette, whose books were full of botanical detail, did not cease gardening even when age and arthritis kept her bedridden. Rather than physical gardens, Colette roamed imagined gardens.
There is nothing so terrible about not having a garden any more. The worrying thing would be if the future garden, whose reality is of no importance, were beyond my grasp. But it is not.
 Colette tended an ‘imagined garden’ when bedridden. Henri Manuel/Wikimedia Commons
Colette tended an ‘imagined garden’ when bedridden. Henri Manuel/Wikimedia CommonsColette planned her “tomorrow garden”, specifying pansies “with wide faces, beards, and moustaches – that look like Henry VIII”. Nothing is too difficult for the imaginative gardener. “An arbour? Naturally I shall have an arbour. I’m not down to my last arbour yet.”
Imagining a garden may seem fanciful. Yet it is less so if considered in the context of embodied semantics – a process where brain connectivity during a thought-about action mirrors the connectivity that occurs during the actual action. (For example, thinking about running or swimming can trigger some of the same neural connections as the physical actions.)
It’s been shown that habitual negativity rewires the brain. Ultimately, it damages it by shrinking the hippocampus: one of the main areas destroyed by Alzheimer’s disease.
But gardens, with their earth-centred sense of time and season, are optimistic places. Watching things grow, deadheading spent flowers and saving seed for the return of spring, are just some of the forward-looking aspects of gardening and perhaps it works as well if the plants and flowers are imagined.
 Gardening can persist throughout an adult life. Centre for Ageing Better/Pexels
Gardening can persist throughout an adult life. Centre for Ageing Better/PexelsIt is logical to go further and ask whether a positive habit, such as imagining a garden, has the potential to help rewire one’s brain in a good way. Imagined gardening is really a form of self-guided imagery, a practice with many applications in the treatment of pain, stress, anxiety and depression.
As we age, ideally we would find ways of getting our hands into the healing soil. Suggestions for gardening in old age, and extreme old age, include introducing raised beds to reduce bending, or working with potted plants.
A friend in her late 70s, with an enviable garden, swears by her Garden Group. Around a dozen friends come together for working bees in each other’s gardens. “You can get a huge amount done in an hour-and-a-half,” she says. Afterwards, they share morning tea – so it is a social as well as practical endeavour. My own best tip is to garden little and often. Committing to half an hour a day, or even 15 minutes, adds up nicely over the course of a week.
American poet May Sarton wrote of gardening as “an instrument of grace”. She regarded the natural world as the great teacher. From the Benedictine Monastery of Saint Paul de Mausole at Saint-Remy-de-Provence, Vincent Van Gogh wrote to his mother: “But for one’s health, as you say, it is very necessary to work in the garden and see the flowers growing.”
Like Monet, Van Gogh needed flowers. We all do. It’s just that many of us forget this during the push and pull of daily life. And in forgetting, we lose touch with our biophilic natures.![]()
Carol Lefevre, Visiting Research Fellow, Department of English and Creative Writing, University of Adelaide
This article is republished from The Conversation under a Creative Commons license. Read the original article.







 Adolescent vaccinations are primarily delivered through school-based programs.
Adolescent vaccinations are primarily delivered through school-based programs.  We need to better understand the barriers to vaccination among adolescents.
We need to better understand the barriers to vaccination among adolescents.  Grapefruit juice may cause some prescription drugs to accumulate in the body.
Grapefruit juice may cause some prescription drugs to accumulate in the body.  The vitamin K in leafy green vegetables, such as kale, may counteract warfarin.
The vitamin K in leafy green vegetables, such as kale, may counteract warfarin. 





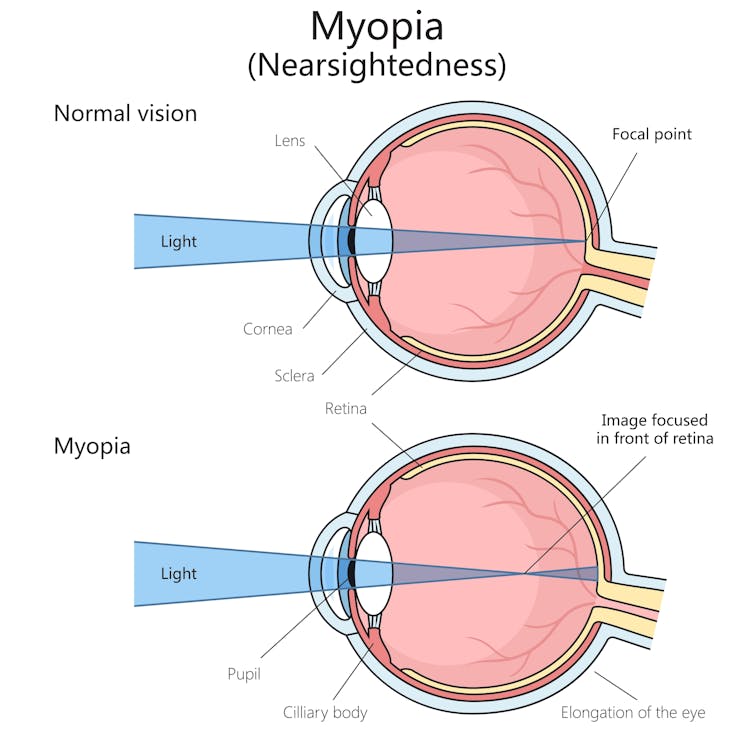 Myopia is a common vision problem.
Myopia is a common vision problem.  Sunlight may play a role in slowing myopia progression.
Sunlight may play a role in slowing myopia progression.  You can monitor your child’s eye health and vision with regular eye tests.
You can monitor your child’s eye health and vision with regular eye tests.